Real-Time Arrhythmia Detection Using Hybrid Convolutional Neural Networks: A Critical Review
Bollepalli et al., Journal of the American Heart Association, 2021
Real-Time Arrhythmia Detection Using Hybrid Convolutional Neural Networks: A Critical Review
Bollepalli et al., Journal of the American Heart Association, 2021
Introduction
ICU monitors track heart rate, blood pressure, oxygen saturation, and respiratory rate and are designed to alert clinical staff of critical events. However, this vigilance comes with a significant and overwhelming 72-99% burden of false alarms.
This creates “alarm fatigue” leading to desensitization of clinical staff to alarms due to their sheer volume and the high proportion of false alarms. Besides annoyance, this has been linked to delayed response times to genuine emergencies, increased patient delirium from noise disturbances, elevated stress for both patients and staff, sleep deprivation, and even patient deaths when critical alarms are ignored or disabled.
The Joint Commission has consistently listed clinical alarm safety as a National Patient Safety Goal since 2012. The study by Bollepalli and colleagues published in the JAHA in December 2021, represents an important contribution to addressing this problem through artificial intelligence and machine learning approaches.
Study Design and Methodology
Data Sources and Population
The investigators used a primary dataset obtained from bedside monitors in the ICUs of Massachusetts General Hospital consisting of 953 independent life-threatening arrhythmia alarms generated from monitors of 410 patients with diverse medical conditions. The data included four channels of electrocardiogram (ECG) signals, arterial blood pressure (BP) waveforms, and photoplethysmograph (PPG) signals.
For external validation, the investigators utilized the publicly available PhysioNet/Computing in Cardiology Challenge 2015 database. This challenge, specifically designed to foster development of algorithms for reducing false arrhythmia alarms, contains 1,250 multi-parameter ICU data segments, each associated with a critical arrhythmia alarm and annotated by expert reviewers as either true or false.
Arrhythmias Under Study
The study focused on detecting six specific rhythm categories: Asystole, Extreme bradycardia (EB), Extreme tachycardia (ET), Ventricular fibrillation (VF), Ventricular tachycardia (VT), and atrial fibrillation (AF).
Ground Truth Establishment
The investigators developed a custom user interface to allow expert annotators to mark the precise onset and offset of both noise segments and arrhythmia episodes across all signal channels. Each record was independently reviewed by two expert annotators, with complex cases adjudicated by a third expert using majority voting. This meticulous approach ensured quality and reliability of training labels.
The authors observed that the alarm type indicated by the bedside monitor frequently did not match the true underlying arrhythmia as determined by expert review. For instance, 22.6% of extreme bradycardia alarms actually corresponded to extreme tachycardia. This observation motivated the investigators’ approach of developing an algorithm that detects arrhythmias without relying on the monitor’s initial alarm classification.
The Hybrid-CNN Architecture: Understanding the Technical Approach
What is a Convolutional Neural Network?
A neural network is a computational model of layers of interconnected processing units that transform input data through a series of mathematical operations to produce an output—in this case, a classification of whether an alarm represents a true arrhythmia or a false alarm. Convolutional neural networks (CNNs) are a specialized type of neural network particularly well-suited for analyzing data with spatial or temporal structure—such as images or, as in this study, physiological waveforms. The key innovation of CNNs is the “convolution” operation: CNNs apply small “filters” that slide across the input, looking for local patterns. For ECG signals, these filters might learn to recognize the characteristic shapes of P waves, QRS complexes, or T waves, or to detect abnormal morphologies associated with specific arrhythmias.
The “deep” in deep learning refers to networks with multiple layers. As data passes through successive layers, the network learns increasingly abstract representations. Early layers might detect simple features like edges or slopes in the ECG waveform; middle layers might combine these into recognizable waveform components; and later layers might integrate these components into holistic assessments of rhythm type.
The Hybrid Approach: Combining Learned and Handcrafted Features
The investigators’ key methodological innovation lies in their “hybrid” approach, which combines two complementary strategies for extracting meaningful information from physiological signals. Traditional machine learning approaches rely on “handcrafted features”—measurements designed by domain experts based on known physiological principles. For arrhythmia detection, these might include heart rate variability measures, the presence or absence of P waves, QRS complex width, or regularity of R-R intervals. Such features encode decades of clinical knowledge about what distinguishes normal from abnormal cardiac rhythms.
In contrast, deep learning approaches using CNNs learn features automatically from the raw data during training. While this can capture subtle patterns that human experts might miss, it also means the network might miss clinically important features that are obvious to trained observers but difficult to learn from limited training data.
The hybrid architecture avoids this trade-off by combining both approaches. The CNN component processes the raw waveform data, learning patterns directly from the signals. Simultaneously, handcrafted features extracted using established signal processing techniques are fed into the network at a later layer. The final classification thus benefits from both the automatic pattern recognition of deep learning and the domain knowledge embedded in traditional features. This fusion occurs at the penultimate layer of the network, just before the final classification output.
Multi-Tiered Classification Strategy
Rather than attempting to classify all arrhythmia types simultaneously, the investigators implemented a hierarchical, multi-tiered approach that mirrors clinical reasoning. Tier-0 serves as a noise detector, identifying signal segments corrupted by artifacts, motion, or electrode problems—channels identified as noisy are masked with zeros and excluded from subsequent analysis. This eliminates noise, the primary source of false alarms in clinical practice.
Tier-1 processes 4-second windows to detect the most immediately life-threatening arrhythmias: ventricular tachycardia and ventricular fibrillation. Tier-2 uses 8-second windows to detect extreme bradycardia and extreme tachycardia, which require longer observation periods to reliably assess heart rate. Finally, Tier-3 distinguishes between atrial fibrillation and sinus rhythm.
This tiered approach prioritizes quick detection of lethal arrhythmias while taking more temporal data for non-critical arrhythmia detection.
Principal Findings and Performance Characteristics
Overall Algorithm Performance
The investigators evaluated their algorithm using 5-fold cross-validation repeated 5 times—a rigorous approach that provides robust estimates of how the algorithm would perform on new, unseen data. The hybrid-CNN model achieved an overall accuracy of 87.5% (±0.5%) and a score of 81.0% (±0.9%). The “score” metric, derived from the PhysioNet Challenge, penalizes false negatives (missed true alarms) five times more heavily than false positives—reflecting the clinical reality that failing to alert clinicians to a genuine life-threatening arrhythmia is far more dangerous than generating an unnecessary alarm.
Importantly, the hybrid approach outperformed both pure CNN-based methods (accuracy 81.2%, score 64.6%) and traditional feature-based methods alone (accuracy 84.3%, score 80.7%). Combining machine learned and handcrafted features provides complementary value and statistically significant improvement (P<0.001) across all tiers.
Performance by Arrhythmia Type
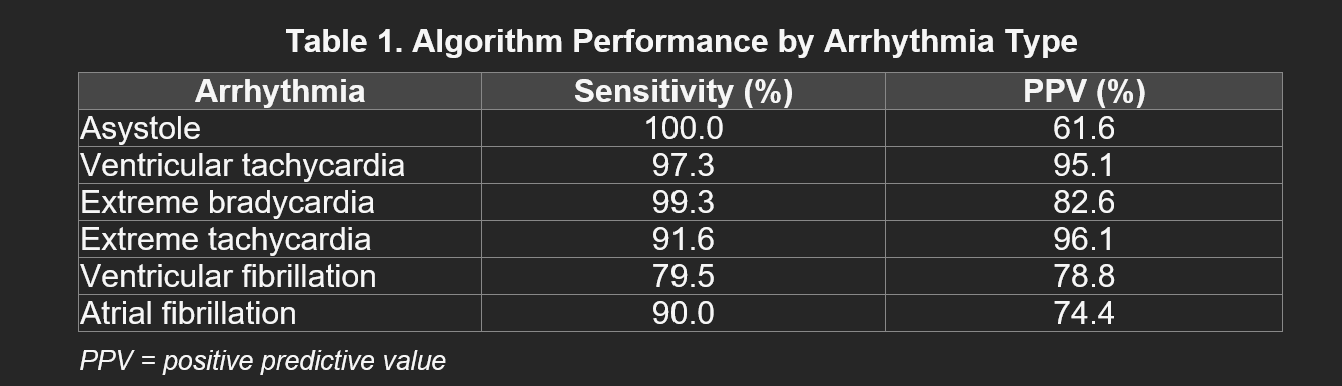
Performance varied across different arrhythmia types, as summarized in Table 1.
Ventricular fibrillation presented more challenges, with 79.5% sensitivity and 78.8% PPV. However, the investigators note an important clinical nuance: all VF events that were “missed” by the algorithm were actually classified as VT. Since both conditions require immediate intervention, this misclassification would not result in delayed treatment.
External Validation Results
External validation of the model on the PhysioNet 2015 Challenge database demonstrated the algorithm’s generalizability. Using only 2-channel ECG (compared to the 4 channels available during training), along with BP and PPG signals, the algorithm achieved 93.9% accuracy and 84.3% score. This score is comparable to the top entries in the original PhysioNet 2015 challenge (85.04%) and represents the highest published score achieved without requiring prior knowledge of the alarm type. The ability to maintain strong performance with reduced input channels demonstrates robustness to real-world conditions where not all signal channels may be available or of adequate quality.
Comparison with Existing Monitoring Systems
In the investigators’ dataset, the monitors generated alarms with a positive predictive value of only 25.29%—i.e., nearly 75% of alarms were false. For specific arrhythmias, the monitor PPVs ranged from 11.3% (asystole) to 53.7% (VT). In contrast, the hybrid-CNN algorithm achieved an average PPV of 82.9% for the five life-threatening arrhythmias, while maintaining sensitivity of 93.5%. Hence, deployment of this algorithm would have suppressed 77.05% of false alarms generated by existing monitors while missing very few true events.
Interpreting the Statistics: What These Numbers Mean in Practice
In a hypothetical ICU with 20 monitored beds, where the current monitoring system generates an average of 350 alarms per bed per day, a false alarm rate of approximately 75% means roughly 5,250 false alarms per day across the unit—or about 220 false alarms per hour, nearly 4 per minute. Each alarm demands attention, interrupts care, and contributes to the noise environment.
If the hybrid-CNN algorithm could suppress 77% of false alarms while maintaining high sensitivity for true events, this would reduce the false alarm burden to approximately 1,200 per day—still substantial, but a dramatic improvement. More importantly, the alarms that do sound would be far more likely to represent genuine clinical events requiring attention, potentially improving response times and reducing the cognitive burden on clinical staff.
Methodological Strengths
First, the rigorous ground truth established with expert annotation and adjudication increases the reliability of the algorithm. Second, the multi-modal approach—integrating ECG, blood pressure, and photoplethysmograph signals—mirrors clinical reasoning by experienced clinicians. The algorithm’s ability to fuse information from multiple sources provides robustness against noise or artifact in any single channel.
Third, external validation on an independent dataset (PhysioNet 2015) demonstrates generalizability beyond the training environment. The algorithm maintained strong performance despite differences in patient populations, monitoring equipment, and signal quality between the two datasets. Fourth, the real-time capability of the algorithm finds clinical relevance. The tiered approach, with 4-second windows for the most urgent arrhythmias and 8-second windows for rate-based diagnoses, allows alerts to be generated with minimal delay—critical for conditions where seconds matter. Fifth, the investigators’ commitment to transparency is noteworthy: they state that both the training dataset and code will be made available to other investigators upon request. This enables independent verification and further development by the research community. This is commendable in this field since most papers do not provide codes for proprietary purposes.
Limitations and Interpretive Cautions
Observational Design
Like most algorithm development studies, this was an observational investigation that assessed predictive accuracy in retrospective data. Whether deploying this algorithm in clinical practice would actually improve patient outcomes remains unanswered.
Population Characteristics and Generalizability
The primary dataset came from a single tertiary academic medical center (Massachusetts General Hospital), which may not represent the diversity of ICU populations nationwide or internationally. External validation on PhysioNet data provides some reassurance, though broader validation remains necessary.
Additionally, the study included only critical arrhythmia alarms. Other types of alarms—for blood pressure, oxygen saturation, respiratory rate, and other parameters—were not addressed.
The Black Box Problem
Deep learning models, including CNNs, are often criticized as “black boxes” because it can be difficult to understand why they make particular predictions. The investigators attempted to address this through gradient-weighted class activation mapping (Grad-CAM), which visualizes which parts of the input signals most influenced the network’s decisions. However, this provides limited insight compared to the interpretability of traditional rule-based systems. The hybrid approach, which incorporates clinically meaningful handcrafted features, may provide more interpretability than pure deep learning methods, but this remains an area for further development.
Sample Size for Rare Events
Some arrhythmia types were represented by relatively few events—for example, only 13 ventricular fibrillation events in the training data. While the investigators used appropriate techniques like cross-validation and the algorithm performed reasonably on VF detection, the limited sample size for rare but critical events introduces uncertainty. Larger datasets with more examples of rare arrhythmias would strengthen confidence in the algorithm’s performance for these conditions.
Contextual Positioning Within the Field
The PhysioNet Challenge Legacy
This study builds upon a substantial body of work catalyzed by the PhysioNet/Computing in Cardiology Challenge 2015. The investigators’ hybrid-CNN approach represents an evolution beyond both traditional methods and early deep learning attempts.
Related Work and Subsequent Developments
Subsequent to this publication, the field has continued to evolve. A 2022 study in Scientific Reports introduced contrastive learning approaches for false alarm reduction, demonstrating that newer deep learning techniques can further improve performance. Systematic reviews published in Frontiers in Digital Health and Exploratory Research and Hypothesis in Medicine have comprehensively catalogued the growing literature on computational approaches to alarm fatigue, finding that while significant progress has been made in algorithm development, translation to clinical practice remains limited.
A 2024 review in BioMedical Engineering OnLine examining deep learning applications in cardiovascular ECG analysis noted the predominance of arrhythmia research in this field, with less attention to other cardiac conditions. The authors observed that public databases like PhysioNet are heavily used in arrhythmia research, while studies of other conditions often rely on proprietary datasets—highlighting the value of the PhysioNet Challenge in driving progress on the alarm fatigue problem.
Clinical Implementation Pathway and Future Directions
Regulatory Considerations
Translation of this algorithm into clinical practice would require regulatory clearance. Robust external validation across diverse populations and settings will be essential for such regulatory approval.
Integration with Clinical Workflows
Successful deployment would require integration with existing monitoring infrastructure, clinical decision support systems, and staff workflows. Questions that must be addressed include: How should the algorithm’s classifications be displayed to clinical staff? Should suppressed alarms be logged for later review? How should staff be trained to understand and appropriately respond to algorithm-assisted alerts?
Systems that generate too many alerts, interrupt workflow, or are perceived as unreliable by clinicians often fail to achieve intended benefits. Human factors engineering and careful attention to the clinician-technology interface will be essential for widespread acceptance and deployment.
The Need for Prospective Trials
The investigators appropriately call for prospective randomized trials to evaluate the clinical efficacy of their approach. Such trials face practical challenges including the need for large sample sizes to detect differences in rare but important outcomes, the difficulty of blinding staff to the intervention, and the potential for Hawthorne effects where simply being studied changes behavior.
Conclusions
The study represents a meaningful advance in the application of artificial intelligence to the problem of false alarms in ICU. Their hybrid approach—combining deep learning with traditional signal processing—achieves strong performance in distinguishing true from false arrhythmia alarms, substantially outperforming existing monitoring systems while maintaining high sensitivity for genuine life-threatening events.
The multi-tiered architecture, multi-modal signal integration, and rigorous validation methodology demonstrate sophisticated engineering combined with clinical insight. External validation on an independent benchmark dataset provides reassurance about generalizability, and the investigators’ commitment to sharing code and data supports scientific reproducibility.
However, as with all AI developments in medicine, there remains a substantial gap between algorithmic performance in research settings and demonstrated clinical benefit. The fundamental question—whether deploying this or similar algorithms will improve patient outcomes in real-world ICUs—awaits prospective clinical trials. The path from promising algorithm to proven intervention requires not only technical refinement but also careful attention to implementation, human factors, and evidence generation.
For clinicians, this study illustrates both the promise and the current limitations of AI in critical care. The technology has advanced to the point where algorithms can match or exceed traditional monitors in distinguishing true from false alarms. Yet the translation of this capability into clinical practice requires the same evidence standards—including randomized controlled trials—that we demand for other medical interventions. The journey from promising prediction to proven benefit continues, but this work represents important progress along that path.
References
1. Bollepalli SC, Sevakula RK, Au-Yeung WM, et al. Real-Time Arrhythmia Detection Using Hybrid Convolutional Neural Networks. J Am Heart Assoc. 2021;10(23):e023222. doi:10.1161/JAHA.121.023222
2. Drew BJ, Harris P, Zègre-Hemsey JK, et al. Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive ICU patients. PLoS One. 2014;9:e110274.
3. Clifford GD, Silva I, Moody B, et al. The PhysioNet/Computing in Cardiology Challenge 2015: Reducing False Arrhythmia Alarms in the ICU. Physiol Meas. 2016;37(8):E5-E23.
4. Au-Yeung WM, Sahani AK, Isselbacher EM, Armoundas AA. Reduction of false alarms in the intensive care unit using an optimized machine learning based approach. NPJ Digit Med. 2019;2:86.
5. Zhou Y, Zhao G, Li J, et al. A contrastive learning approach for ICU false arrhythmia alarm reduction. Sci Rep. 2022;12:4689.
6. Chromik J, Klopfenstein SAI, Pfitzner B, et al. Computational approaches to alleviate alarm fatigue in ICU medicine: A systematic literature review. Front Digit Health. 2022;4:843747.
7. Huo JY, et al. Reducing False Alarms in ICU: A Scoping Review. Explor Res Hypothesis Med. 2023;8(1):56-68.
8. Keller JP. Clinical alarm hazards: a “top ten” health technology safety concern. J Electrocardiol. 2012;45:588-591.
9. Hannun AY, Rajpurkar P, Haghpanahi M, et al. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat Med. 2019;25:65-69.
10. Winters BD, Cvach MM, Bonafide CP, et al. Technological Distractions (Part 2): A Summary of Approaches to Manage Clinical Alarms With Intent to Reduce Alarm Fatigue. Crit Care Med. 2018;46(1):130-137.


Wow. Whats about false negatives? So smart, thanks!